Our Strathfield location has now closed permanently.
For existing follow up and new patient referrals, please see our other Sydney practices:
Dr John Chang
EASTWOOD
www.eastwoodeye.com.au
02 8188 2020
Dr Mark Gorbatov and Dr Kwon Kang
SYDNEY CBD
www.retinavitreous.com.au
02 9223 8880
Uveitis
Uveitis is a group of eye diseases whereby the middle layer of the eyeball called the “uvea” gets inflamed (red and swollen). Uveitis can affect all age groups from children, and young adults to older persons. It can cause acutely painful red eye or more gradual onset of visual difficulties including blurred vision and floaters.

Image from WebMD: A visual guide to uveitis
Uveitis can cause a wide range of symptoms that can come on quickly over a few days, to more gradual onset over weeks and months. It can affect one or both eyes. Symptoms can include:
- Having a red eye, with or without pain
- Being very sensitive to bright light
- Blurry vision or acute loss of eyesight
- Seeing “floaters” (shaped like specks or cobwebs moving in your vision)
- Seeing “flashes” of light
Uveitis can be described by its temporal nature: acute uveitis typically has an abrupt onset of a painful red eye, whilst chronic uveitis may present more insidiously with a gradual onset of blurred vision without necessarily any associated eye pain.
Uveitis is further classified into 4 main types by eye specialists, according to the main site that is inflamed within the eye:
1. Anterior uveitis: Inflammation affects the front part of the eye (iris) and usually has acute onset of symptoms with painful red eye occurring within days. Anterior uveitis is by far the most common type of uveitis.
2. Intermediate uveitis: involves inflammation of the uvea in the middle part of the eye. It usually has symptoms that are more gradual in onset with worsening floaters and blurred vision. The eye may not necessarily be red or painful.
3. Posterior uveitis: affects the back of the eye (retina, choroid, optic nerve) and most cases are sight-threatening.
4. Panuveitis: This is the most serious form of uveitis that affects all layers of the eye from the front to the back.
Under each of the above types of uveitis, there are many specific uveitis diagnoses that are known by other names (eg. Fuch’s heterochromic iridocyclitis, herpetic uveitis, or toxoplasma chorioretinitis). By far the most common type of uveitis in Australia is acute anterior uveitis or “iritis”.[1]
1. John Chang, Denis Wakefield. Uveitis: a global perspective. Ocular Immunology & Inflammation 2002;10:263-279.
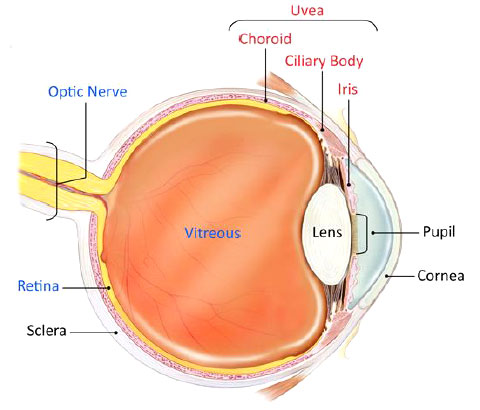
Image from National Eye Institute: Facts about uveitis
Uveitis is often caused by a disturbance in the body’s immunity and so can be seen on its own or in association with other autoimmune conditions such as inflammatory bowel disease, multiple sclerosis, or rheumatologic conditions such as arthritis and lupus. [2]
Some forms of uveitis are caused by infections such as herpes virus, syphilis, tuberculosis and parasites such as toxoplasmosis. In some cases, despite extensive investigations, no known cause is found (so called “idiopathic uveitis”).
2. John Chang, Peter McCluskey, Denis Wakefield. Acute anterior uveitis and HLA-B27. Survey of Ophthalmology 2005;50:364-388.
An eye doctor (ophthalmologist) will examine the eye from the front to the back using specialised equipments in the clinic to detect the pattern of uveitis as well as its severity. Uveitis can cause vision loss in various ways including causing a cataract, glaucoma, swelling at the back of the eye (macula), or retinal damage. The ophthalmologist will carefully look for all of these potential complications.
Uveitis needs to be treated promptly to prevent lasting problems, pain or loss of eyesight. Treatment varies depending on the type and severity of the uveitis, hence the importance of an accurate diagnosis. Ophthalmologists often treat uveitis with eye drop medicine that reduces inflammation (corticosteroids). Sometimes, in sight-threatening cases, medicines may need to be given by injections around or into the eye, or by oral tablets. Uveitis caused by infections need appropriate antibiotic or antiviral medicines. It is important for such treatments to be administered and supervised by the ophthalmologist to prevent blinding complications.
Patients with uveitis may also develop associated eye conditions such as cataract and glaucoma. These need expert attention and treatments may involve carefully timed cataract, glaucoma and retinal surgery.
Uveitis may affect not only the eye, but it can occur in the context of infective or immune conditions that affect other parts of the body such as the lungs, joints, bowels or skin. As a consequence, the ophthalmologist may look after patients with uveitis as part of a team with other specialist doctors such as rheumatologist, immunologist or respiratory physician.